The study of a series of patients at Madigan Army Medical Center here, has led doctors to discover a new unique sleep-related condition impacting combat Soldiers called Trauma-associated Sleep Disorder.
“Redeployed military personnel have reported for the last 13 years complex nighttime behaviors ranging from sleepwalking, tossing and turning, thrashing, screaming, and even hitting their bed partners,” said Col. (Dr.) Vincent Mysliwiec, principal investigator and lead author, and U.S. Army Medicine sleep medicine specialist. “While these disruptive nocturnal behaviors are frequently reported, they are rarely documented in laboratory settings.”
Although previous authors recognized some of the unique sleep disturbances seen in combat survivors, the constellation of findings of disruptive nocturnal behaviors, nightmares and rapid eye movement, or REM, sleep without atonia had never been linked together. There was no current diagnosis which encompassed all these trauma engendered sleep disturbances.
Atonia is also known as sleep paralysis, which occurs when a person suddenly finds himself or herself unable to move for a few minutes, most often upon falling asleep or waking up. Sleep paralysis is due to an irregularity in passing between the stages of sleep and wakefulness.
“Up until this time, it was unknown what military personnel and trauma survivors had in terms of a clinical disorder,” said Mysliwiec. “In many cases they were diagnosed with nightmare disorder, which does not have movements associated with this diagnosis, or REM Behavior Disorder, which occurs in middle-aged to elderly males and has a characteristic clinical presentation. This case series highlights the unique findings of TSD (Trauma-associated Sleep Disorder).”
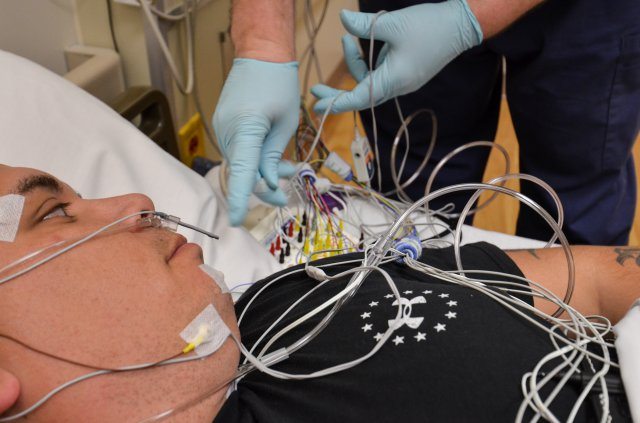
The case series included four Soldiers who had been evaluated, diagnosed and treated at Madigan. Each Soldier underwent a clinical evaluation in the hospital’s sleep medicine clinic and was given an attended, overnight polysomnogram (sleep study). The polysomnogram recorded body functions, such as heart rate, brain waves, movements and any sounds they made during sleep.
According to published results, all of the young men developed disruptive nighttime behaviors and nightmares after suffering a traumatic experience. Some reported screaming and combative movements, while others experienced night sweats and crying episodes throughout the night.
“Normally individuals in REM sleep are paralyzed and do not move, thus they are unable to act out their dreams. Patients with TSD appear to have dream enactment, with purposeful movements that can occur in REM sleep,” said Mysliwiec. “This case series is a major step forward in not only diagnosis and treatment of military personnel with sleep disturbances, but also sleep safety for families.”
In addition to providing trauma survivors with the understanding that they have a clinical diagnosis, this case study also helps facilitate future research in the sleep disturbances that develop after trauma.
“Better characterization of the clinical findings is required, especially in regards to the onset of TSD and how much REM without atonia is present,” said Mysliwiec. “Prospective studies are required to evaluate treatment regimens, as many service members and veterans have findings of TSD.”
This case series appears online and in print this month in the Journal of Clinical Sleep Medicine, the official publication of the American Academy of Sleep Medicine.