Since 2000, more than 2,000 servicemembers have suffered amputated limbs. DARPA’s breakthrough research with advanced prosthetic limbs controlled by brain interfaces is well documented, but such research is currently limited to quadriplegics; practical applications of brain interfaces for amputees are still in the future.
In contrast, nerve and muscle interfaces allow amputees to control advanced prosthetics in the near term. Recent demonstrations may give Wounded Warriors hope that they can soon take advantage of these breakthroughs.
DARPA’s Reliable Neural-Interface Technology (RE-NET) program researched the long-term viability of brain interfaces and continues research to develop high-performance, reliable peripheral interfaces.
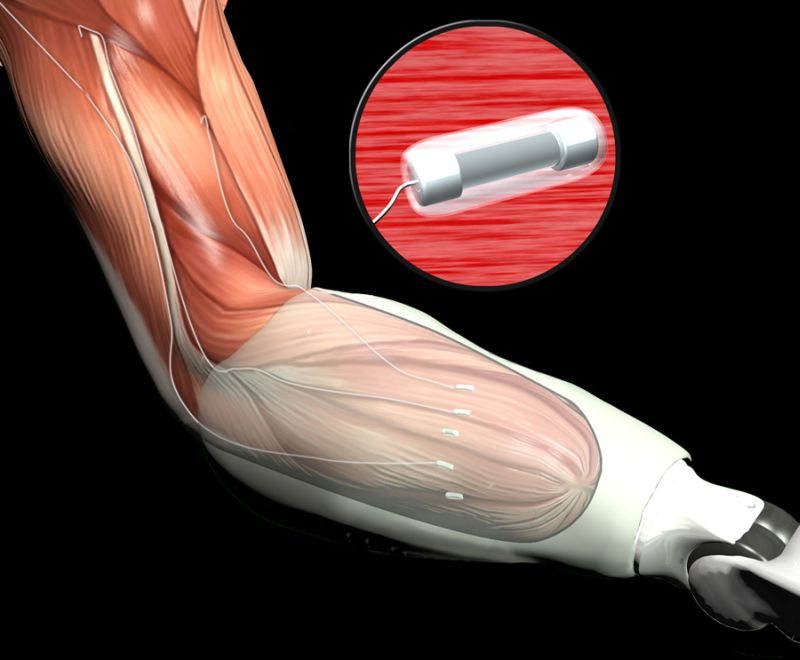
These new peripheral interfaces use signals from nerves or muscles to both control prosthetics and to provide direct sensory feedback. Ongoing clinical trials present compelling examples of both interface types.
“Although the current generation of brain, or cortical, interfaces have been used to control many degrees of freedom in an advanced prosthesis, researchers are still working on improving their long-term viability and performance,” said Jack Judy, DARPA program manager.
“The novel peripheral interfaces developed under RE-NET are approaching the level of control demonstrated by cortical interfaces and have better biotic and abiotic performance and reliability.
“Because implanting them is a lower risk and less invasive procedure, peripheral interfaces offer greater potential than penetrating cortical electrodes for near-term treatment of amputees. RE-NET program advances are already being made available to injured warfighters in clinical settings.”
A team of researchers at the Rehabilitation Institute of Chicago (RIC) demonstrated a type of peripheral interface called targeted muscle re-innervation (TMR). By rewiring nerves from amputated limbs, new interfaces allow for prosthetic control with existing muscles.
Former Army Staff Sgt. Glen Lehman, injured in Iraq, recently demonstrated improved TMR technology. In the following video, Lehman demonstrates simultaneous joint control of a prosthetic arm made possible by support from the RE-NET program.
Researchers at Case Western Reserve University used a flat interface nerve electrode (FINE) to demonstrate direct sensory feedback. By interfacing with residual nerves in the patient’s partial limb, some sense of touch by the fingers is restored. Other existing prosthetic limb control systems rely solely on visual feedback.
Unlike visual feedback, direct sensory feedback allows patients to move a hand without keeping their eyes on it-enabling simple tasks, like rummaging through a bag for small items, not possible with today’s prosthetics.
The Case Western Reserve University video shows how direct sensory feedback makes some tasks easier. The FINE is one of many different types of nerve interfaces developed under the RE-NET program.
“With the RE-NET program, DARPA took on the mission of giving our wounded vets increased control of advanced prosthetics,” added Judy.
“TMR is already being used by numerous amputees at military hospitals. As the RE-NET program continues, we expect that the limb-control and sensory-feedback capabilities of peripheral-interface technologies will increase and that they will become even more widely available in the future.”
DARPA’s current efforts with peripheral interfaces are scheduled to continue up to 2016.